Antiviral with Immune Booster Therapy: Current concept for clinical care in Covid-19
DOI:
https://doi.org/10.21760/jaims.8.4.10Keywords:
Immunotherapy, Rasayana, Anti-viral herbs, Kalaja Bala, Cosmic immunity.Abstract
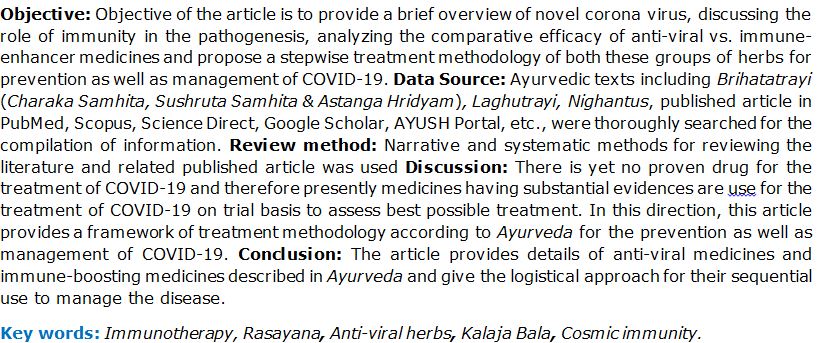
Objective: Objective of the article is to provide a brief overview of novel corona virus, discussing the role of immunity in the pathogenesis, analyzing the comparative efficacy of anti-viral vs. immune- enhancer medicines and propose a stepwise treatment methodology of both these groups of herbs for prevention as well as management of COVID-19. Data Source: Ayurvedic texts including Brihatatrayi (Charaka Samhita, Sushruta Samhita & Astanga Hridyam), Laghutrayi, Nighantus, published article in PubMed, Scopus, Science Direct, Google Scholar, AYUSH Portal, etc., were thoroughly searched for the compilation of information. Review method: Narrative and systematic methods for reviewing the literature and related published article was used Discussion: There is yet no proven drug for the treatment of COVID-19 and therefore presently medicines having substantial evidences are use for the treatment of COVID-19 on trial basis to assess best possible treatment. In this direction, this article provides a framework of treatment methodology according to Ayurveda for the prevention as well as management of COVID-19. Conclusion: The article provides details of anti-viral medicines and immune-boosting medicines described in Ayurveda and give the logistical approach for their sequential use to manage the disease.
Downloads
References
Roujian Lu, Xiang Zhao, Juan Li, Peihua Niu, Bo Yang, et.al. Genomic characterization and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020; 395: 565–574.
Coronaviridae Study Group of the International Committee on Taxonomy of Viruses. The species severe acute respiratory syndrome related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. 2020; 5: 536–544.
Yu Chen, Lanjuan Li. SARS-CoV-2: virus dynamics and host response. Lancet. Infect. Dis. 2020;20(5):515-516.
Di Wu, Tiantian Wu, Qun Liu, Zhicong Yang. The SARS-CoV-2 outbreak: What we know. Int. J. Infect. Dis. 2020; 94: 44-48.
Chih C Lai, Tzu P Shih , Wen C Ko , Hung J Tang , Po R Hsueh. Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) and Coronavirus disease-2019 (COVID-19): The Epidemic and the Challenges. Int. J. Antimicrob. Agents. 2020;55(3):105924.
Zhixin Liu, Xiao Xiao, Xiuli Wei, Jian Li, Jing Yang, Huabing Tan, et. al. Composition and divergence of coronavirus spike proteins and host ACE2 receptors predict potential intermediate hosts of SARS‐CoV‐2. J. Med. Virol. 2020; 92 (6):595-601.
M. Ceccarelli, M. Berretta, E. Venanzi Rullo, G. Nunnari, B. Cacopardo. Differences and similarities between Severe Acute Respiratory Syndrome (SARS)-CoronaVirus (CoV) and SARS-CoV-2. Would a rose by another name smell as sweet?. Eur. Rev. Med. Pharmacol Sci. 2020; 24(5): 2781-2783.
Su L, Ma X, Yu H, et al. The different clinical characteristics of corona virus disease cases between children and their families in China - the character of children with COVID-19. Emerg. Microbes. Infect. 2020; 9(1):707‐713.
Zheng J. SARS-CoV-2: an Emerging Coronavirus that Causes a Global Threat. Int. J. Biol. Sci. 2020;16(10):1678‐1685.
Guo YR, Cao QD, Hong ZS, Tan YY, Chen SD, Jin HJ, et.al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak - an update on the status. Mil. Med. Res. 2020;7(1):11.
Li YC, Bai WZ, Hashikawa T. The neuroinvasive potential of SARS-CoV2 may play a role in the respiratory failure of COVID-19 patients. J. Med. Virol. 2020; 92(6):552-555.
Klimstra WB, Heidner HW, Johnston RE. The furin protease cleavage recognition sequence of Sindbis virus PE2 can mediate virion attachment to cell surface heparan sulfate. J. Virol. 1999;73(8):6299‐6306.
Belouzard S, Millet JK, Licitra BN, Whittaker GR. Mechanisms of coronavirus cell entry mediated by the viral spike protein. Viruses. 2012;4(6):1011‐1033.
Belouzard S, Chu VC, Whittaker GR. Activation of the SARS coronavirus spike protein via sequential proteolytic cleavage at two distinct sites. Proc. Natl. Acad. Sci. 2009;106(14):5871-6.
Alexandra C.Walls, Young-Jun Park, M. Alejandra Tortoric, Abigail Wall Andrew T.McGuire, David Veesler. Structure, Function, and Antigenicity of the SARS-CoV-2 Spike Glycoprotein. Cell. 2020;181(2): 281-292.
Wu Z, Mc Googan JM. Characteristics of and Important Lessons from the Coronavirus Disease 2019 (COVID-19) Outbreak in China: summary of a Report of 72314 Cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020; 323(13):1239-1242.
Bagi HM, Soleimanpour M, Abdollahi F, Soleimanpour H. Evaluation of clinical outcomes of patients with mild symptoms of coronavirus disease 2019 (COVID-19) discharged from the emergency department. 2021. PloS One. 16(10): e0258697.
Blair JE, Gotimukul A, Wang F, Mina SA, et. al. Mild to moderate COVID-19 illness in adult outpatients: Characteristics, symptoms, and outcomes in the first 4 weeks of illness. Medicine (Baltimore). 2021; 100(24):e26371.
Yuki K, Fujiogi M, Koutsogiannaki S. COVID-19 pathophysiology: A review. Clin. Immunol. 2020; 215:108427.
Hussin AR, Siddappa NB. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J. Autoimmun. 2020; 109: 102433.
Cao W, Li T. COVID-19: towards understanding of pathogenesis. Cell. Res. 2020; 30:367–369.
Patwardhan B, Chavan GP, Gautam M, Tillu G, et.al. Ayurveda rasayana in prophylaxis of COVID-19. Current Science. 2020; 118 (8): 1158-1160.
Gu J Korteweg C. Pathology and pathogenesis of severe acute respiratory syndrome. Am. J. Pathol. 2007;170(4):1136‐1147.
Tay MZ, Poh CM, Renia L. et al. The trinity of COVID-19: immunity, inflammation and intervention. Nat. Rev. Immunol. 2020;20: 363–374.
Rajput ZI, Hu SH, Xiao CW, Arijo AG. Adjuvant effects of saponins on animal immune responses. J. Zhejiang. Univ. Sci. B. 2007;8(3):153‐161.
Charaka Samhita, Sutrasthana, Kriyantshirishyadhya, 17/117. Available from: http://niimh.nic.in/ebooks/ ecaraka/?mod=read. [Last accessed on 2021 April 10].
Saha S, Ghosh S. Tinospora cordifolia: One plant, many roles. Anc. Sci. Life. 2012;31(4):151‐159.
Sharma U, Bala M, Kumar N, Singh B, Munshi RK, Bhalerao S. Immunomodulatory active compounds from Tinospora cordifolia. J. Ethnopharmacol. 2012; 141(3):918-26.
Gupta R, Sharma V. Ameliorative effects of tinospora cordifolia root extract on histopathological and biochemical changes induced by aflatoxin-b(1) in mice kidney. Toxicol. Int. 2011;18(2):94-8.
Sharma V, Pandey D. Beneficial Effects of Tinospora cordifolia on Blood Profiles in Male Mice Exposed to Lead. Toxicol. Int. 2010; 17(1):8-11.
Rege A A Anil, Chowdhary A Sadashiv. Evaluation of Ocimum sanctum and Tinospora cordifolia as Probable HIV-Protease Inhibitors. Int. J. Pharm. Sci. Rev. Res. 2014;25(1): 315-318
Sachan S, Dhama K, Shyma KL, Samad HA, Mariappan AK, et.al. Immunomodulatory Potential of Tinospora cordifolia and CpG ODN (TLR21 Agonist) against the Very Virulent, Infectious Bursal Disease Virus in SPF Chicks. Vaccines. 2019; 7:106.
Wu Y, Li J, Kim Y. et al. In vivo and in vitro antiviral effects of berberine on influenza virus. Chin. J. Integr. Med. 2011;17: 444–452.
Srinivasan GV, Unnikrishnan KP, Rema Shree AB, Balachandran I. HPLC Estimation of berberine in Tinospora cordifolia and Tinospora sinensis. Indian. J. Pharm. Sci. 2008;70(1):96‐99.
Narayanan AS, Raja SS, Ponmurugan K, Kandekar SC, Natarajaseenivasan K, Maripandi A, Mandeel QA. Antibacterial activity of selected medicinal plants against multiple antibiotic resistant uropathogens: a study from Kolli Hills, Tamil Nadu, India. Benef. Microbes. 2011; 2(3):235-43.
Thatte UM, Kulkarni MR, Dahanukar SA. Immunotherapeutic modification of Escherichia coli peritonitis and bacteremia by Tinospora cordifolia. J. Postgrad. Med. 1992; 38(1):13-5.
Suresh K, Vasudevan DM. Augmentation of murine natural killer cell and antibody dependent cellular cytotoxicity activities by Phyllanthus emblica, a new immunomodulator. J. Ethnopharmacol. 1994; 44(1):55-60.
Xiang Y, Pei Y, Qu C, et.al. In vitro anti-herpes simplex virus activity of 1,2,4,6-tetra-O-galloyl-β-D-glucose from Phyllanthus emblica L. (Euphorbiaceae). Phytother. Res. 2011; 25(7):975-82.
Qing L, Ya-Feng W, Rong-Jie C, Mei-Ying Z, Yi-Fei W, et.al. Anti-Coxsackie Virus B3 Norsesquiterpenoids from the Roots of Phyllanthus emblica. J. Nat. Prod. 2009; 72( 5): 969-972.
Jun-jiang L, Ya-Feng W, Jing-Min Z, Shan Yu, Hong-Tao Z, et.al. Anti Hepatitis B Virus Activities and Absolute Configurations of Sesquiterpenoid Glycosides from Phyllanthus emblica. Org. Biomol. Chem. 2014; 12: 1-10.
JunJiang L, ShanYu, Ying Xin, et. al. Anti-viral and cytotoxic norbisabolane sesquiterpenoid glycosides from Phyllanthus emblica and their absolute configurations. Phytochem. 2015; 117:123-134.
Narges B, Mohammad H K, Zahra A. The effect of glycyrrhizin on maturation and T cell stimulating activity of dendritic cells. Cell Immunol. 2012; 280(1): 44-49.
Jose C, Pierre VA, LenkaT, et.al. Free radical-scavenging, antioxidant and immunostimulating effects of a licorice infusion (Glycyrrhiza glabra L.). Food Chem. 2010; 122(1): 508-517
Hoever G, Baltina L, Michaelis M, et. al. Antiviral activity of glycyrrhizic acid derivatives against SARS-coronavirus. J. Med. Chem. 2005; 48(4):1256-9.
Pompei R, Pani A, Flore O, Marcialis MA, Loddo B. Antiviral activity of glycyrrhizic acid. Experientia. 1980; 36(3):304.
Badam L. In vitro antiviral activity of indigenous glycyrrhizin, licorice and glycyrrhizic acid (Sigma) on Japanese encephalitis virus. J. Commun. Dis. 1997; 29(2):91-99.
Cristina F, Michael E, Rea K , Eugenio R, Donatella P, et.al. Antiviral effects of Glycyrrhiza species. Phytother. Res. 2008; 22(2):141-148.
Kesharwani A, Polachira SK, Nair R, Agarwal A, Mishra NN, Gupta SK. Anti-HSV-2 activity of Terminalia chebula Retz extract and its constituents, chebulagic and chebulinic acids. BMC Complement. Altern. Med. 2017;17(1):110.
Lin LT, Chen TY, Chung CY, Noyce RS, et.al. Hydrolyzable tannins (chebulagic acid and punicalagin) target viral glycoprotein-glycosaminoglycan interactions to inhibit herpes simplex virus 1 entry and cell-to-cell spread. J. Virol. 2011; 85(9) :4386-98.
Krishnasamy, Rajamaheswari T, Anand Baba, et.al. In Silico Analysis of Active Compounds from Siddha Herbal Infusion of Ammaiyar Koondhal Kudineer (Akk) Against SARS-CoV-2 Spike Protein and Its ACE2 Receptor Complex. 2020; SSRN: https://ssrn.com/abstract=3578294 or http://dx.doi.org/10.2139/ssrn.3578294
Shivaprasad HN, Kharya MD, Rana AC, S Mohan. Preliminary Immunomodulatory Activities of the Aqueous Extract of Terminalia chebula. Pharm. Biol. 2006; 44(1): 32-34.
Sharma R, Martins N, Kuca K, et al. Chyawanprash: A Traditional Indian Bioactive Health Supplement. Biomolecules. 2019; 9(5):161.
Sastry JLN, Gupta Arun, Brindavanam NB, Kanjilal S, Kumar S et.al. Quantification of Immunity Status of Dabur Chyawanprash - A Review Part- 2 (Clinical Studies). Indian J. Appl. Res. 2011; 4(3): 205-211.
Gupta A, Kumar S, Dole S, et al. Evaluation of Cyavanaprasa on Health and Immunity related Parameters in Healthy Children: A Two Arm, Randomized, Open Labeled, Prospective, Multicenter, Clinical Study. Anc. Sci. Life. 2017; 36(3):141-150.
N Uma, Dhananjay S Kotasthane. A Cytogenetic Study on the Efficacy of Chyawanprash Awaleha as an Antioxidant in Oral Premalignant Cancer. J. Oral Oncol. 2014;5: 864230.
Goothy SS. Effect of Chyawanprash on cognitive, autonomic and respiratory parameters in college students. Int. J. Res. Ayurveda Pharm. 2014; 5:435-438.
Poudel S, Pradeep, Yadav MP. Agastya Haritaki Rasayana: A Critical Review. Journal of Drug Delivery and Therapeutics. 2019; 9(1-s):486-91.
Patil U. Studies on Antiviral Activity of Tulsi (Ocimum sanctum) crude extracts on selected viruses of veterinary importance. Int. J. Ayurveda Pharm. Res. 2018; 6(4):17-21.
Ghoke SS, Sood R, Kumar N. et al. Evaluation of antiviral activity of Ocimum sanctum and Acacia arabica leaves extracts against H9N2 virus using embryonated chicken egg model. BMC Complement. Altern. Med. 2018;18(1): 174.
Nahak G, Sahu R K. Immunostimulatory effect of Ocimum sanctum Linn. leaf extract in Clarias batrachus Linn. International Journal of Pharmacy and Pharmaceutical Sciences. 2014; 6(6):157-163.
Mandal S, Verma S, Vishwa D B, Satya Narayan N, et. al, Double-blinded randomized controlled trial for immunomodulatory effects of Tulsi (Ocimum sanctum Linn.) leaf extract on healthy volunteers. J Ethnopharmacol. 2011; 136(3): 452-456.
Panda VS, Suresh RN. Evaluation of cardioprotective activity of Ginkgo biloba and Ocimum sanctum in rodents. Altern. Med. Rev. 2009;14(2):161-71.
Badam L, Bedekar SS, Sonawane KB, Joshi SP. In vitro antiviral activity of Bael (Aegle marmelos Corr) upon human coxsackieviruses B1-B6. J. Commun. Dis. 2002;34(2):88-99.
Badam L, Joshi SP, Bedekar SS. In vitro antiviral activity of neem (Azadirachta indica. A. Juss) leaf extract against group B coxsackieviruses. J. Commun. Dis. 1999; 31(2):79-90.
Ligia C, Faccin G, Kristie A, Yamamoto, Ray S, et. al. The in vitro antiviral property of Azadirachta indica polysaccharides for poliovirus. J. Ethnopharmacol. 2012; 142(1): 86-90.
Parida MM, Upadhyay C , Pandya G, Jana AM . Inhibitory potential of neem (Azadirachta indica Juss) leaves on Dengue virus type-2 replication. J. Ethnopharmacol. 2002; 79(2): 273-278.
Weber ND, Andersen DO, North JA, Murray BK, Lawson LD, Hughes BG. In vitro virucidal effects of Allium sativum (garlic) extract and compounds. Planta. Med. 1992; 58(5):417-23.
Mehrbod P, Amini E, Kheiri M. Antiviral activity of garlic extract on Influenza virus. 2009; Iranian. J. Virol. 3:19-23.
Masato N, Kayo K, Jun Ichiro S, Yukihiro K. Antimicrobial properties of hydrophobic compounds in garlic: Allicin, vinyldithiin, ajoene and diallyl polysulfides. Exp. Ther. Med. 2019; 8388: 1550-1553
Ali Y, Kerem C, Ergin M A. Comparison of Antimicrobial Activity of Allium sativum Cloves from China and Taskopru, Turkey. Nature-Inspired Drugs: Expanding Horizons of Contemporary Therapeutics. 2018 ; 9302840 .
Jonkers D, Sluimer J, Stobberingh E. Effect of garlic on vancomycin-resistant enterococci. Antimicrob. Agents Chemother. 1999;43(12):30-45.
Yoshida H, Katsuzaki H, Ohta R, et al. Antimicrobial activity of the thiosulfinates isolated from oil-macerated garlic extract. Biosci. Biotechnol. Biochem. 1999; 63(3):591–594.
Moutia M, Habti N, Badou A. In Vitro and In Vivo Immunomodulator Activities of Allium sativum L. eCAM. 2018; 4984659.
Arreola R, Quintero F S, Lopez Roa RI, et al. Immunomodulation and anti-inflammatory effects of garlic compounds. J. Immunol. Res. 2015;401630.