Effect of Neutral Pulmonary Douche on Pulmonary Functions among Bronchial Asthma Patients
DOI:
https://doi.org/10.21760/jaims.9.3.6Keywords:
Hydrotherapy, Douche, Pulmonary Function, Spirometry, Bronchial AsthmaAbstract
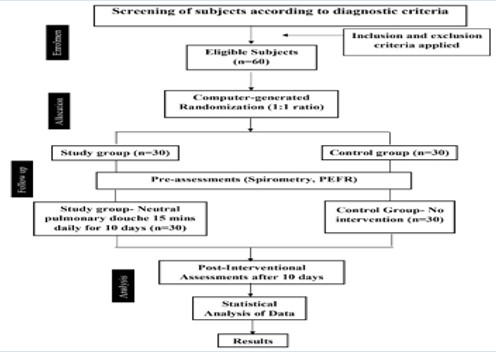
Introduction: Bronchial Asthma is the second-most significant contributing factor to mortality rates for chronic respiratory diseases. It is characterized by hyperreactivity of the airways and reversible episodes of bronchoconstriction. Douche is a general application in hydrotherapy, which is a stream of water directed against the body generally or locally. The neutral pulmonary douche (NPD) is employed to improve pulmonary functions, but there is no scientific report validating its effect. Materials and Method: A randomized control trial study of a total of 60 subjects belonging to the age group of 18–44 years participated in the study. The study participants were randomized into intervention and control groups (1:1). The intervention group (30) underwent NPD for 30 minutes. No intervention was given to the control group (30) and was followed up. The assessments were taken at baseline and after 10 days of the study. Result: The collected data was subjected to statistical analysis, employing interferential statistical tests. These analyses showed a significant difference in all parameters (FEV1, FVC, the FEV1FVC ratio, and PEFR) within (t-tests, the Wilcoxon rank test) and between (ANCOVA) groups. Conclusion: The implementation of hydrotherapy-facilitated NPD has demonstrated notable enhancement of pulmonary functionality in Bronchial asthma (BA) sufferers, in conjunction with conventional medical interventions. This discovery contributes to the progressively accumulating substantiation endorsing the efficacy of hydrotherapy within the domain of naturopathy.
Downloads
References
G., M., Cochrane., William, Jackson., John, Rees., John, O, Warner. Asthma: Current Perspectives. (1996).
Smith AD, Cowan JO, Filsell S, et al. Diagnosing asthma: comparisons between exhaled nitric oxide measurements and conventional tests. Am J Respir Crit Care Med. 2004;169(4):473-478. doi:10.1164/rccm. 200310-1376OC.
Cao Y, Chen S, Chen X, et al. Global trends in the incidence and mortality of asthma from 1990 to 2019: An age-period-cohort analysis using the global burden of disease study 2019. Front Public Health. 2022 Nov 22;10:1036674. doi: 10.3389/fpubh.2022.1036674. PMID: 36483262; PMCID: PMC9723391.
J., C., Virchow. [Asthma - historical development, current status and perspectives]. Pneumologie, (2010).;64(09):541-549. doi: 10.1055/S-0030-1255695
Swati, Y, Bhave., Harish, K, Pemde. Current management: asthma. Apollo Medicine, (2005).;2(4):334-341. doi: 10.1016/S0976-0016(11)60517-6
Jamshid, Salamzadeh. Asthma: Achievements and Questions in Front. Iranian Journal of Pharmaceutical Sciences, (2005).;1(2):63-76.
Karen Angus., Michael Parsons., Neil Cheeseman, et al. Asthma Exacerbation: An Emergency Medicine Simulation Scenario. Cureus, (2015).;7(3) doi: 10.7759/CUREUS.258
Atta Abbas., Sadaf Shahid., Arif Sabah, et al. The Clinical Complications of Asthma and its Pharmacotherapy. British Biomedical Bulletin, (2014).;2(1):117-146.
Sheikh Rayees., Inshah Din. Current Asthma Treatments. (2021).19-25. doi: 10.1007/978-3-030-70270-0_7
Woo-Jung Song., Ji Hyang Lee., Yewon Kang, et al. Future Risks in Patients with Severe Asthma. Allergy, Asthma and Immunology Research, (2019).;11(6):763-778. doi: 10.4168/AAIR.2019.11.6.763
Patrick Lefebvre., Mei Sheng Duh., Marie-Hélène, et al. Burden of systemic glucocorticoid-related complications in severe asthma. Current Medical Research and Opinion, (2017).;33(1):57-65. doi: 10.1080/03007995.2016.1233101.
Aidan A., Long. The burden of asthma and improving patient outcomes. The American Journal of Managed Care, (2011).;17
Patricia A., Loftus., Sarah K, et al. Epidemiology and economic burden of asthma. International Forum of Allergy & Rhinology, (2015).;5 doi: 10.1002/ALR.21547
Peng Zhou., Leiming Xi., Hongan He., et al. A comparison of efficacy and safety of complementary and alternative therapies for children with asthma: A protocol for systematic review and meta-analysis. Medicine, (2021).;100(11) doi: 10.1097/MD.0000000000024946
Eun Ji Kim., Eun Ji Kim., Joseph Simonson, et al. Disparities in complementary alternative medicine use and asthma exacerbation in the United States. Journal of Asthma, (2020).;57(8):866-874. doi: 10.1080/02770903.2019.1614615
Anca Maierean., Lorena Ciumărnean., Teodora Alexescu, et al. Complementary therapeutic approaches in asthma. (2019).;10:204-212. doi: 10.12680/BALNEO.2019.258.
Therapeutic Benefits of Naturopathy Douches in Hydrotherapy. (2022).10-15. doi: 10.9734/jocamr/2022 /v17i430337
Porjadkov, Leonid, Fedorovich. Douche-hydraulic massaging apparatus. (2008).
Samuel R., Meaker. The vaginal douche. JAMA, (1926).;87(17):1377-1379. doi: 10.1001/JAMA.1926.0268017 0031010
Alexander K S, Ballard. Portable douche and sitz bath. (1974).
Gary, L., Plyant Bidet, douche and enema system. (2002).
Pavithira M. Immediate effect of alternate douche to whole body on autonomic and respiratory variables in healthy volunteers. 2020;6(5):541–4.
Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention, 2021. Definition, description, and diagnosis of asthma, Chapter-1. 2021. P-23. Available from: www.ginasthma.org, GINA Full Report 2021 Front Cover ONLY (ginasthma.org).
Dr. J.H. Kellogg. Rational Hydrotherapy. Douche: Pulmonary douche. 3rd edition. NIN, Pune. 2016. p.508-9.
Harpreet Ranu, Michael Wilde, Brendan Madden. Pulmonary Function Tests. The Ulster Medical Journal. 2011; 80(2):84-90. PMID: 22347750, PMCID: PMC3229853.
Kroegel C. (2007). Krankheitskontrolle als Therapieprinzip beim Asthma bronchiale [Global Initiative for Asthma Management and Prevention--GINA 2006]. Pneumologie (Stuttgart, Germany), 61(5), 295–304. https://doi.org/ 10.1055/s-2007-959180
Bousquet J., Khaltaev N., Cruz A. A., et al (2008). Allergic Rhinitis and its Impact on Asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA (2)LEN and AllerGen). Allergy, 63 Suppl 86, 8–160. https://doi.org/10.1111/j.1398-9995.2007.01620.x
Liu Y-C, Khawaja A, Rogers D. Pathophysiology of airway mucus secretion in asthma. Asthma: Elsevier; 1998. p. 205-27. 10.1016/B978-012079027-2/50093-9.
Digiesi V, Cerchiai G, Mannini L, et al. Modificazioni emoreologiche ed ematiche nell'uomo in corso di immersione parziale, con metodo terapeutico, in acqua a 38 degrees C [Hemorheologic and blood cell changes in humans during partial immersion, with a therapeutic method, in 38 C water]. Minerva Med. 1986;77(30-31):1407-1411. PMID: 3736976.
Chen E, Miller GE. Stress and inflammation in exacerbations of asthma. Brain Behav Immun. 2007 Nov;21(8):993-9. doi: 10.1016/j.bbi.2007.03.009. Epub 2007 May 9. PMID: 17493786; PMCID: PMC2077080.
Giesbrecht, G. G., & Younes, M. (1995). Exercise- and cold-induced asthma. Canadian journal of applied physiology = Revue canadienne de physiologie appliquee, 20(3), 300–314. https://doi.org/10.1139/h95-023.