Study of Aama and Dysbiosis for Future Microbiological and Biotechnological Advancement in Ayurveda - Case Controlled Literary Study
DOI:
https://doi.org/10.21760/jaims.9.10.35Keywords:
Aama, dysbiosis, biotechnology, microbiologyAbstract
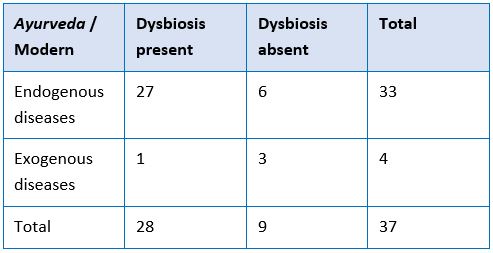
Introduction: In Ayurveda there are various concepts that require special attention due to their complex nature and lack of understanding of human mind. One such concept is Aama that is so far considered as toxins or free radicles in body. Our limited understanding in advance sciences like biotechnology has limited us to understand these complex yet highly valuable concepts. Through this study we will try to understand Aama in the reference of gut biota dysbiosis and disease progression. Aim: To understand Aama in perspective of dysbiosis and establishing its direct relation with advance microbiological and biotechnological researches. Methodology: Study of major pathological conditions where Aama is involved, Study of affected biota and toxins (if involved/studied) in those conditions. And further evaluation using statistical test. Discussion: Such studies in the segment of Ayurveda can lead to understand the mechanism of various functional dynamics of body as described in Ayurveda. This can be helpful in developing the concepts further and enhance our understanding toward complexity of human body. Future of this study can be seen as complete understanding of this concept of Aama. Further using biotechnological tools we can develop investigations module for confirming presence or amount of Aama present in cell or body. Further studies in medicine can help us rule out the most appropriate medicines for various pathological groups of organisms.
Downloads
References
Martín Giménez VM, Modrego J, Gómez-Garre D, et al. Gut Microbiota Dysbiosis in COVID-19: Modulation and Approaches for Prevention and Therapy. Int J Mol Sci. 2023 Jul 31; 24(15):12249. doi: 10.3390/ijms241512249. PMID: 37569625; PMCID: PMC10419057.
Shuyun Xu, Zhenzhen Liu, Meihua Lv, Yuli Ch, Intestinal dysbiosis promotes epithelial-mesenchymal transition by activating tumor-associated macrophages in ovarian cancer, Pathogens and Disease, Volume 77, Issue 2, March 2019, ftz019, https://doi.org/10.1093/femspd/ftz019
Zhou Zheng, Sun Bao, Yu Dongsheng, Zhu Chunshen, Gut Microbiota: An Important Player in Type 2 Diabetes Mellitus, Frontiers in Cellular and Infection Microbiology, vol12, 2022, https://www.frontiersin.org/articles/10.3389/fcimb.2022.834485 doi: 10.3389/fcimb.2022.834485, 2235-2988
Buhaș MC, Gavrilaș LI, Candrea R, Cătinean A, Mocan A, Miere D, Tătaru A. Gut Microbiota in Psoriasis. Nutrients. 2022 Jul 20; 14(14):2970. doi: 10.3390/nu14142970. PMID: 35889927; PMCID: PMC9321451.
Eribo, O.A., du Plessis, N., Ozturk, M. et al. The gut microbiome in tuberculosis susceptibility and treatment response: guilty or not guilty? Cell. Mol. Life Sci. 77, 1497–1509 (2020). https://doi.org/10.1007/s00018-019-03370-4
Fattorusso A, Di Genova L, Dell'Isola GB, et al. Autism Spectrum Disorders and the Gut Microbiota. Nutrients. 2019 Feb 28; 11(3):521. doi: 10.3390/nu11030521. PMID: 30823414; PMCID: PMC6471505.
Chatzikonstantinou, S, Gioula, G, Kimiskidis, VK, et al. The gut microbiome in drug-resistant epilepsy. Epilepsia Open. 2021; 6: 28–37. https://doi.org/10.1002/epi4.12461
Saint-Criq V, Lugo-Villarino G, Thomas M. Dysbiosis, malnutrition and enhanced gut-lung axis contribute to age-related respiratory diseases. Ageing Res Rev. 2021 Mar; 66:101235. doi: 10.1016/j.arr.2020.101235. Epub 2020 Dec 13. PMID: 33321253.
Lobo LA, Benjamim CF, Oliveira AC. The interplay between microbiota and inflammation: lessons from peritonitis and sepsis. Clin Transl Immunology. 2016 Jul 15; 5(7):e90. doi: 10.1038/cti.2016.32. PMID: 27525063; PMCID: PMC4973320.
Lobo LA, Benjamim CF, Oliveira AC. The interplay between microbiota and inflammation: lessons from peritonitis and sepsis. Clin Transl Immunology. 2016 Jul 15; 5(7):e90. doi: 10.1038/cti.2016.32. PMID: 27525063; PMCID: PMC4973320.
Palumbo VD, Tutino R, and Messina M, et al. Altered Gut Microbic Flora and Haemorrhoids: Could They Have a Possible Relationship? J Clin Med. 2023 Mar 12; 12(6):2198. doi: 10.3390/jcm12062198 . PMID: 36983199; PMCID: PMC10054427.
Wei, L., Singh, R., Ro, S. and Ghoshal, U.C. (2021), Gut microbiota dysbiosis in functional gastrointestinal disorders: Underpinning the symptoms and pathophysiology. JGH Open, 5: 976-987. https://doi.org/10.1002/jgh3.12528
Ananya FN, Ahammed MR, Fahem MM, et al. Association of Intestinal Microbial Dysbiosis with Chronic Obstructive Pulmonary Disease. Cureus. 2021 Nov 7; 13(11):e19343. doi: 10.7759/cureus.19343. PMID: 34909304; PMCID: PMC8653930.
Wei, L., Singh, R., Ro, S. and Ghoshal, U.C. (2021), Gut microbiota dysbiosis in functional gastrointestinal disorders: Underpinning the symptoms and pathophysiology. JGH Open, 5: 976-987. https://doi.org/10.1002/jgh3.12528
Wei, L., Singh, R., Ro, S. and Ghoshal, U.C. (2021), Gut microbiota dysbiosis in functional gastrointestinal disorders: Underpinning the symptoms and pathophysiology. JGH Open, 5: 976-987. https://doi.org/10.1002/jgh3.12528
Saint-Criq V, Lugo-Villarino G, Thomas M. Dysbiosis, malnutrition and enhanced gut-lung axis contribute to age-related respiratory diseases. Ageing Res Rev. 2021 Mar; 66:101235. doi: 10.1016/j.arr.2020.101235. Epub 2020 Dec 13. PMID: 33321253.
Day AW, Kumamoto CA. Gut Microbiome Dysbiosis in Alcoholism: Consequences for Health and Recovery. Front Cell Infect Microbiol. 2022 Mar 3; 12:840164. D¬oi: 10.3389/fcimb.2022.840164. PMID: 35310839; PMCID: PMC8928144.
Awasthi, Ankit, Corrie, et al, Gut Dysbiosis and Diabetic Foot Ulcer: Role of Probiotics vl- 14, Pharmaceutics, 2022/11/21; 2543, doi - 10.3390/pharmaceutics14112543
Yin J, Liao SX, He Y, Wang S, Xia GH, Liu FT, Zhu JJ, You C, Chen Q, Zhou L, Pan SY, Zhou HW. Dysbiosis of Gut Microbiota with Reduced Trimethylamine-N-Oxide Level in Patients with Large-Artery Atherosclerotic Stroke or Transient Ischemic Attack. J Am Heart Assoc. 2015 Nov 23; 4(11):e002699. doi: 10.1161/JAHA.115.002699. PMID: 26597155; PMCID: PMC4845212.
Shi Z, Qiu Y, Wang J, et al Dysbiosis of gut microbiota in patients with neuromyelitis optica spectrum disorders: A cross sectional study. J Neuroimmunol. 2020 Feb 15; 339:577126. doi: 10.1016/j.jneuroim.2019.577126. Epub 2019 Dec 9. PMID: 31841737
Kandpal M, Indari O, Baral B, et al. Dysbiosis of Gut Microbiota from the Perspective of the Gut-Brain Axis: Role in the Provocation of Neurological Disorders. Metabolites. 2022 Nov 3; 12(11):1064. doi: 10.3390/metabo12111064. PMID: 36355147; PMCID: PMC9692419.
Romero-Figueroa María del Socorro,Ramírez-Duran Ninfa, et al, Gut-joint axis: Gut dysbiosis can contribute to the onset of rheumatoid arthritis via multiple pathways, Frontiers in Cellular and Infection Microbiology,13,2023, https://www.frontiers.org/articles/10.3389/fcimb.2023.1092118 , 10.3389/fcimb.2023.1092118, 2235-2988
López-Moreno A, Aguilera M. Vaginal Probiotics for Reproductive Health and Related Dysbiosis: Systematic Review and Meta-Analysis. J Clin Med. 2021 Apr 2; 10(7):1461. doi: 10.3390/jcm10071461. PMID: 33918150; PMCID: PMC8037567.
Scibelli N, Singh P, Raynor K. Intestinal Dysbiosis Disguised as a Rectal Fistula Treated With Autologous Fecal Microbiota Transplantation. Cureus. 2021 Mar 25; 13(3):e14115. doi: 10.7759/cureus.14115. PMID: 33927926; PMCID: PMC8075766.
Yuan, T., Xia, Y., Li, B. et al. Gut microbiota in patients with kidney stones: a systematic review and meta-analysis. BMC Microbiol 23, 143 (2023). https://doi.org/10.1186/s12866-023-02891-0
Dongxin, Zhang, Huang, Yinping, Ye, Duyun, Intestinal dysbiosis: An emerging cause of pregnancy complications? Medical Hypotheses 84, 2015/01/09, 10.1016/j.mehy.2014.12.029
Zhang J, Xia Y, Sun J. Breast and gut microbiome in health and cancer. Genes Dis. 2020 Aug 20; 8(5):581-589. doi: 10.1016/j.gendis.2020.08.002. PMID: 34291130; PMCID: PMC8278537.
Knezevic J, Starchl C, Tmava Berisha A, Amrein K. Thyroid-Gut-Axis: How Does the Microbiota Influence Thyroid Function? Nutrients. 2020 Jun 12; 12(6):1769. doi: 10.3390/nu12061769. PMID: 32545596; PMCID: PMC7353203.
Madra M, Ringel R, Margolis KG. Gastrointestinal Issues and Autism Spectrum Disorder. Child Adolesc Psychiatr Clin N Am. 2020 Jul; 29(3):501-513. doi: 10.1016/j.chc.2020.02.005. Epub 2020 Apr 2. PMID: 32471598; PMCID: PMC8608248.
Minodier L, Masse S, Capai L, et al. Clinical and virological factors associated with gastrointestinal symptoms in patients with acute respiratory infection: a two-year prospective study in general practice medicine. BMC Infect Dis. 2017 Nov 22; 17(1):729. doi: 10.1186/s12879-017-2823-9. PMID: 29166867; PMCID: PMC5700681.
Dr. Ram Manohar P, Lecture on 'Aama-Dosha-Sthana (ADS) System of Diagnosis, Ayurveda network VHU, https://youtu.be/yIRAFfGlGcY?si=Y7aw5lqtWRK1MpId