A Statistical Analysis of Om Jap Dhyan on Anxiety Level
DOI:
https://doi.org/10.21760/jaims.10.9.5Keywords:
Om Jap Dhyan, anxiety, elderly people, virtual, Samadhi, Sinha’s Comprehensive Anxiety Test, neurophysiologicalAbstract
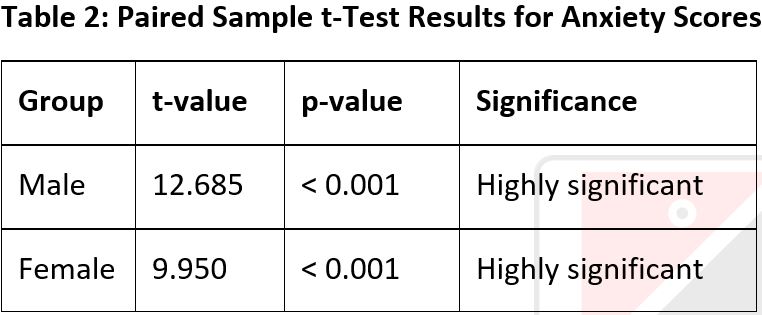
The main aim of this research article is to present the outcomes of the Om Jap Dhyan particularly on mental problem; anxiety within the male and female to the elderly peoples and to interpret the results in statistical analysis. Actually, the Om Jap Dhyan is virtual program running in the evening time since 2019 A.D in covid time conducted by Om Jap Dhyan Samiti under the guidance of Patanjali Yog Samiti Lumbini Pradesh, Nepal. It includes three types of meditations and the same number of Sutras of Rishi Patanjali's Yog Darshan. The 27th Sutra of Samadhi Pad "Tasyavachakahpranavah" is named as Om Chanting Meditation, 35th sutra of Samadhi Pad “Vishayavativa Pravritti Utpannamanasah Sthitini Bandhani” is named as Music Meditation and 51st Sutra of Sadhanpada Bāhyābhyantara-Viṣaya-Ākṣepīcaturthaḥ" is named as Pran Meditation. This study investigates the impact of Om Jap Dhyan on anxiety level among elderly peoples, focusing on 25 males and 25 females’ participants aged 50 to 70 years. Using a pre-post research design, they are divided into two groups: males and females. Both groups are engaged daily in evening time for Om Jap Dhyan practice continuously in one month altogether 40 minutes in which Om Chanting meditation for 20 minutes, Music Meditation for 10 minutes and Pran Meditation for 10 minutes. Anxiety levels are measured before and after the intervention using Depression Anxiety Stress Scales (DASS). The results reveals significant reductions in anxiety for both genders, with experiencing a greater decrease in males compared to females. Statistical analysis showed highly significant t-values (male group: t = 12.685, female group: t = 9.950) and significance levels (p< 0.001) for both groups. The quantitative analysis suggests that Om Jap Dhyan is an effective method for reducing anxiety in elderly peoples and highlights its potential as a complementary therapy to conventional treatments.
Downloads
References
Crawford JR, Henry JD. The Depression Anxiety Stress Scales (DASS): Normative data and latent structure in a large non-clinical sample. Br J Clin Psychol. 2003;42(2):111–31. https://doi.org/10.1348/014466503321903544
Beekman ATF, Bremmer MA, Deeg DJH, van Balkom AJLM, Smit JH, de Beurs E, et al. Anxiety disorders in later life: A report from the Longitudinal Aging Study Amsterdam. Int J Geriatr Psychiatry. 1998;13(10):717–26. https://doi.org/10.1002/(SICI)1099-1166(1998100)13:10<717::AID-GPS847>3.0.CO;2-E
Wolitzky-Taylor KB, Castriotta N, Lenze EJ, Stanley MA, Craske MG. Anxiety disorders in older adults: A comprehensive review. Depress Anxiety. 2010;27(2):190–211. https://doi.org/10.1002/da.20653
Telles S, Sharma SK, Singh N. Sound-based meditation practices: Mechanisms and benefits. J Complement Integr Med. 2018;15(3). https://doi.org/10.1515/jcim-2017-0072
Innes KE, Selfe TK, Alexander GK. Meditation and neuroplasticity: A review of the current literature. Brain Cogn. 2016;105:15–23. https://doi.org/10.1016/j.bandc.2016.03.007
Bera TK, Jain R, Das T. Effect of Om chanting on anxiety and emotional well-being: A randomized controlled trial. Indian J Psychol Ment Health. 2017;11(2):85–92.
Mahapatra S, Jha A. Om chanting as a stress management technique: A controlled trial on professionals. Asian J Psychiatry. 2020;50:101980. https://doi.org/10.1016/j.ajp.2020.101980
Shankaran S, Pillai S, Rao H. A meta-analytic review of mantra-based meditation for anxiety: Evidence from 2010–2022. Mindfulness. 2023;14(2):345–59. https://doi.org/10.1007/s12671-023-02043-0
Telles S, Gupta RK, Yadav A, Balkrishna A. EEG changes during Om chanting: Meditation versus repetition of a neutral syllable. Int J Yoga. 2015;8(1):3–6. https://doi.org/10.4103/0973-6131.146046
Kalyani BG, Venkatasubramanian G, Arasappa R, Rao NP, Kalmady SV, Behere RV, et al. Neurohemodynamic correlates of ‘OM’ chanting: A pilot functional magnetic resonance imaging study. Int J Yoga. 2016;4(1):3–6. https://doi.org/10.4103/0973-6131.66770
Bhargav H, Srinivasan TM, Shankaranarayana Rao BS. Heart rate variability changes during Om chanting in anxiety-prone individuals. Int J Yoga. 2021;14(1):22–8. https://doi.org/10.4103/ijoy.IJOY_48_20
Rathod S, Mehta V. The efficacy of Om chanting as an adjunct to CBT in the treatment of generalized anxiety disorder. J Integr Ment Health. 2022;8(1):19–26.
Singh M, Dubey S. Om meditation as an emotional regulation tool in geriatric anxiety: A field study in care homes. Indian J Geriatr Psychiatry. 2019;35(3):220–6.
Joshi R, Prakash R. Impact of Om chanting meditation on occupational stress among corporate employees. J Occup Health Psychol. 2018;23(3):311–20. https://doi.org/10.1037/ocp0000109
Bradt J, Dileo C. Music interventions for mechanically ventilated patients. Cochrane Database Syst Rev. 2016;9:CD006902. https://doi.org/10.1002/14651858.CD006902.pub3
Lin YJ, Lee TM, Yeh ML. Effects of music listening and music meditation on anxiety in adults: A randomized controlled trial. Complement Ther Med. 2018;41:300–6. https://doi.org/10.1016/j.ctim.2018.09.007
de Witte M, Spruit A, van Hooren S, Moonen X, Stams GJ. Effects of music interventions on stress-related outcomes: A meta-analysis. Trends Psychol. 2020;28(3):632–51. https://doi.org/10.1007/s43076-020-00033-7
Bradt J, Teague A. Music interventions for anxiety in adults: A systematic review. Arts Psychother. 2019;62:54–62. https://doi.org/10.1016/j.aip.2019.101611
Nilsson U. The effect of music meditation on preoperative anxiety: A randomized controlled trial. J Perianesth Nurs. 2021;36(1):25–30. https://doi.org/10.1016/j.jopan.2020.03.004
Koelsch S. Brain correlates of music-evoked emotions. Nat Rev Neurosci. 2017;18(3):170–80. https://doi.org/10.1038/nrn.2017.1
Tang YY, Tang R, Posner MI. Brief music-based mindfulness meditation improves emotion regulation and neuroplasticity: An fMRI study. Soc Cogn Affect Neurosci. 2020;15(3):234–43. https://doi.org/10.1093/scan/nsz098
Goldberg SB, Meyer B, Davidson RJ. Music meditation in clinical anxiety: A randomized pilot study. J Clin Psychol. 2021;77(2):345–57. https://doi.org/10.1002/jclp.23044
Sima N, Wu L, Guo J. Music meditation and occupational stress among healthcare professionals during COVID-19: A longitudinal intervention study. Int J Occup Health. 2022;78(4):412–20. https://doi.org/10.1007/s13478-022-00213-z
Zhang H, Wang Y. The effects of music meditation on anxiety and depression in elderly adults: A quasi-experimental study. Geriatr Nurs. 2019;40(6):627–33. https://doi.org/10.1016/j.gerinurse.2019.03.014
Sengupta P. Health impacts of Pran Meditation and yogic breathing: A narrative review. J Ayurveda Integr Med. 2016;7(4):251–8. https://doi.org/10.1016/j.jaim.2016.07.001
Sharma A, Bansal P, Khatri S. Effectiveness of Pran Meditation on anxiety and self-efficacy among college students. Indian J Health Wellbeing. 2017;8(5):442–5.
Telles S, Singh N, Balkrishna A. Managing mental health disorders through yogic breathing: Pran Meditation for anxiety reduction. Front Psychiatry. 2018;9:707. https://doi.org/10.3389/fpsyt.2018.00707
Patel S, Kulkarni D. Comparing mindfulness-based stress reduction and Pran Meditation for anxiety relief: A randomized study. Mindfulness. 2022;13(1):89–101. https://doi.org/10.1007/s12671-021-01766-3
Nivethitha L, Mooventhan A, Manjunath NK. Physiological effects of slow breathing: A review on Pran Meditation and vagal stimulation. J Clin Psychol. 2020;76(3):432–41. https://doi.org/10.1002/jclp.22854
Desai R, Mehta R. Neural correlates of Pran Meditation: A functional MRI study on anxiety reduction. Neurosci Lett. 2021;765:136200. https://doi.org/10.1016/j.neulet.2021.136200
Gupta P, Kumar R, Singh M. Effect of Pran Meditation on cortisol levels and anxiety symptoms in adults: A pilot study. Indian J Psychol Med. 2019;41(2):122–7. https://doi.org/10.4103/IJPSYM.IJPSYM_158_18
Mishra S, Kaur H, Joshi P. A pilot study on the effects of Pran Meditation on adults with generalized anxiety disorder. Asian J Psychiatry. 2020;53:102207. https://doi.org/10.1016/j.ajp.2020.102207
Deshpande S, Bhatt A. Online Pran Meditation program for frontline workers during COVID-19: A quasi-experimental study. J Occup Health Psychol. 2021;26(4):425–35. https://doi.org/10.1037/ocp0000301
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Prem Shah, V. K. Katiyar, Narayan Prasad Pahari, Dinesh Panthi

This work is licensed under a Creative Commons Attribution 4.0 International License.