Exploring the relationship between Gut Dysbiosis and Acne Vulgaris in Adolescence and Young Adults: A Narrative Review
DOI:
https://doi.org/10.21760/jaims.10.2.24Keywords:
Acne vulgaris, Gut Dysbiosis, Gut - skin axis, Naturopathy treatmentAbstract
Acne vulgaris is a common skin condition, particularly in adolescents and young adults, resulting from clogged hair follicles due to excess sebum and dead skin cells. While its causes include genetic, hormonal, and environmental factors, recent research suggests gut dysbiosis plays a significant role in acne development. This review examines the connection between gut microbiota imbalance and acne, focusing on the gut-skin axis, where disruptions in the gut microbiome can trigger systemic inflammation and affect skin health. Dysbiosis may compromise both the gut and skin barriers, contributing to acne through inflammation, altered lipid metabolism, and immune dysfunction. Factors like diet, antibiotics, and stress can worsen this imbalance. Interventions such as probiotics, prebiotics, and dietary changes show promise in managing acne by restoring gut health and reducing inflammation. This review also highlights the importance of understanding the gut-skin axis in acne treatment and alternative therapies such as acupuncture, herbal medicine, and naturopathic approaches in managing acne vulgaris. Further research is needed to elucidate the exact mechanisms and therapeutic potentials of gut-skin interactions in acne management.
Downloads
References
Chilicka K, Dzieńdziora-Urbińska I, Szyguła R, Asanova B, Nowicka D. Microbiome and probiotics in acne vulgaris—A narrative review. Life. 2022 Mar 15;12(3):422.
Salem I, Ramser A, Isham N, Ghannoum MA. The gut microbiome as a major regulator of the gut-skin axis. Front Microbiol. 2018 Jul 10;9:1459.
Baglama ŠŠ, Trčko K. Skin and gut microbiota dysbiosis in autoimmune and inflammatory skin diseases. Acta Derm Alp Pannonica Adriat. 2022 Sep;31:105-9.
Belkaid Y, Hand TW. Role of the microbiota in immunity and inflammation. Cell. 2014 Mar 27;157(1):121-41.
Helander HF, Fändriks L. Surface area of the digestive tract—revisited. Scand J Gastroenterol. 2014 Jun 1;49(6):681-9.
Mahmud MR, Akter S, Tamanna SK, Mazumder L, Esti IZ, Banerjee S, Akter S, Hasan MR, Acharjee M, Hossain MS, Pirttilä AM. Impact of gut microbiome on skin health: gut-skin axis observed through the lenses of therapeutics and skin diseases. Gut Microbes. 2022 Dec 31;14(1):2096995.
Guarner F, Khan AG, Garisch J, Eliakim R, Gangl A, Thomson A, Krabshuis J, Lemair T, Kaufmann P, De Paula JA, Fedorak R. World Gastroenterology Organisation global guidelines: probiotics and prebiotics October 2011. J Clin Gastroenterol. 2012 Jul 1;46(6):468-81.
Renz H, Brandtzaeg P, Hornef M. The impact of perinatal immune development on mucosal homeostasis and chronic inflammation. Nat Rev Immunol. 2012 Jan;12(1):9-23.
Grice EA, Segre JA. The skin microbiome. Nat Rev Microbiol. 2011;9(4):244-53.
De Pessemier B, Grine L, Debaere M, Maes A, Paetzold B, Callewaert C. Gut-skin axis: current knowledge of the interrelationship between microbial dysbiosis and skin conditions. Microorganisms. 2021 Feb 11;9(2):353.
Mohiuddin AK. Acne protection: measures and miseries. Dermatol Clin Res. 2019;5(1):272-311.
Yan HM, Zhao HJ, Guo DY, Zhu PQ, Zhang CL, Jiang W. Gut microbiota alterations in moderate to severe acne vulgaris patients. J Dermatol. 2018 Oct;45(10):1166-71.
Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, Shibuya K, Salomon JA, Abdalla S, Aboyans V, Abraham J. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012 Dec 15;380(9859):2163-96.
Katsuta Y, Iida T, Inomata S, Denda M. Unsaturated fatty acids induce calcium influx into keratinocytes and cause abnormal differentiation of epidermis. J Invest Dermatol. 2005 May 1;124(5):1008-13.
Suh DH, Kwon HH. What's new in the physiopathology of acne? Br J Dermatol. 2015 Jul;172:13-9.
Sánchez-Pellicer P, Navarro-Moratalla L, Núñez-Delegido E, Ruzafa-Costas B, Agüera-Santos J, Navarro-López V. Acne, microbiome, and probiotics: the gut-skin axis. Microorganisms. 2022 Jun 27;10(7):1303.
Grice EA, Kong HH, Conlan S, Deming CB, Davis J, Young AC, Bouffard GG, Blakesley RW, Murray PR, Green ED. Topographical and temporal diversity of the human skin microbiome. Science. 2009 May 29;324(5931):1190-2.
Zaenglein AL, Pathy AL, Schlosser BJ, Alikhan A, Baldwin HE, Berson DS, Bowe WP, Graber EM, Harper JC, Kang S, Keri JE. Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol. 2016 May 1;74(5):945-73.
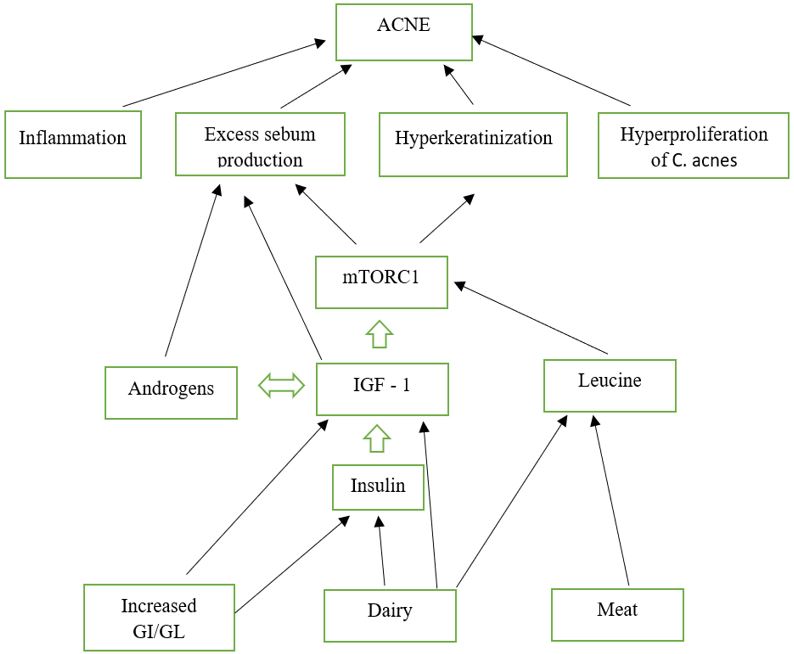
Melnik B. Dietary intervention in acne: attenuation of increased mTORC1 signaling promoted by Western diet. Dermatoendocrinol. 2012 Jan 1;4(1):20-32.
Smith TM, Gilliland K, Clawson GA, Thiboutot D. IGF-1 induces SREBP-1 expression and lipogenesis in SEB-1 sebocytes via activation of the phosphoinositide 3-kinase/Akt pathway. J Invest Dermatol. 2008 May 1;128(5):1286-93.
Wolkenstein P, Misery L, Amici JM, Maghia R, Branchoux S, Cazeau C, Voisard JJ, Taïeb C. Smoking and dietary factors associated with moderate-to-severe acne in French adolescents and young adults: results of a survey using a representative sample. Dermatology. 2015 Nov 19;230(1):34-9.
Baldwin H, Tan J. Effects of diet on acne and its response to treatment. Am J Clin Dermatol. 2021 Jan;22:55-65.
Nair PMK, Salwa H, Satyalakshmi K. Clinical naturopathy: a manual for physicians and students. Pune: National Institute of Naturopathy; 2017. ISBN:978-81-9326-72-0-6.
Noureldein MH, Eid AA. Gut microbiota and mTOR signaling: insight on a new pathophysiological interaction. Microb Pathog. 2018 May 1;118:98-104.
Vojvodic A, Peric-Hajzler Z, Matovic D, Vojvodic P, Vlaskovic-Jovicevic T, Sijan G, Dimitrijevic S, Stepic N, Wollina U, Badr BA, Badawi A. Gut microbiota and the alteration of immune balance in skin diseases: from nutraceuticals to fecal transplantation. Open Access Maced J Med Sci. 2019 Sep 9;7(18):3034.
LeBlanc JG, Milani C, De Giori GS, Sesma F, Van Sinderen D, Ventura M. Bacteria as vitamin suppliers to their host: a gut microbiota perspective. Curr Opin Biotechnol. 2013 Apr 1;24(2):160-8.
Mahmud MR, Akter S, Tamanna SK, Mazumder L, Esti IZ, Banerjee S, Akter S, Hasan MR, Acharjee M, Hossain MS, Pirttilä AM. Impact of gut microbiome on skin health: gut-skin axis observed through the lenses of therapeutics and skin diseases. Gut Microbes. 2022 Dec 31;14(1):2096995.
Deepa Y. Integrative yoga and naturopathy approach to managing acne vulgaris: a single case study.
Belkaid Y, Harrison OJ. Homeostatic immunity and the microbiota. Immunity. 2017 Apr 18;46(4):562-76.
Goto Y, Panea C, Nakato G, Cebula A, Lee C, Diez MG, Laufer TM, Ignatowicz L, Ivanov II. Segmented filamentous bacteria antigens presented by intestinal dendritic cells drive mucosal Th17 cell differentiation. Immunity. 2014 Apr 17;40(4):594-607.
Lyte M. Microbial endocrinology and the microbiota-gut-brain axis. Microbial Endocrinol. 2014 Jun 9:3-24.
Langan EA, Lisztes E, Bíró T, Funk W, Kloepper JE, Griffiths CE, Paus R. Dopamine is a novel, direct inducer of catagen in human scalp hair follicles in vitro. Br J Dermatol. 2013 Mar 1;168(3):520-5.
Guo X, Li J, Tang R, Zhang G, Zeng H, Wood RJ, Liu Z. High-fat diet alters gut microbiota and the expression of Paneth cell-antimicrobial peptides preceding changes of circulating inflammatory cytokines. Mediators Inflamm. 2017;2017(1):9474896.
Lee YB, Byun EJ, Kim HS. Potential role of the microbiome in acne: a comprehensive review. J Clin Med. 2019 Jul 7;8(7):987.
Dall’Oglio F, Nasca MR, Fiorentini F, Micali G. Diet and acne: review of the evidence from 2009 to 2020. Int J Dermatol. 2021 Jun;60(6):672-85.
Dreno B, Gollnick HP, Kang S, Thiboutot D, Bettoli V, Torres V, Leyden J. Global Alliance to Improve Outcomes in Acne. Understanding innate immunity and inflammation in acne: implications for management. J Eur Acad Dermatol Venereol. 2015 Jun;29:3-11.
Melnik B. Dietary intervention in acne: attenuation of increased mTORC1 signaling promoted by Western diet. Dermatoendocrinol. 2012 Jan 1;4(1):20-32.
Ansaldo E, Farley TK, Belkaid Y. Control of immunity by the microbiota. Annu Rev Immunol. 2021 Apr 26;39(1):449-79.
Spencer EH, Ferdowsian HR, Barnard ND. Diet and acne: a review of the evidence. Int J Dermatol. 2009 Apr 1;48(4).
Block SG, Valins WE, Caperton CV, Viera MH, Amini S, Berman B. Exacerbation of facial acne vulgaris after consuming pure chocolate. J Am Acad Dermatol. 2011 Oct 1;65(4):e114-5.
Costa A, Lage D, Moisés TA. Acne and diet: truth or myth? An Bras Dermatol. 2010;85:346-53.
Kaymak Y, Adisen E, Ilter N, Bideci A, Gurler D, Celik B. Dietary glycemic index and glucose, insulin, insulin-like growth factor-I, insulin-like growth factor binding protein 3, and leptin levels in patients with acne. J Am Acad Dermatol. 2007 Nov 1;57(5):819-23.
Forsythe CE, Phinney SD, Fernandez ML, Quann EE, Wood RJ, Bibus DM, Kraemer WJ, Feinman RD, Volek JS. Comparison of low-fat and low-carbohydrate diets on circulating fatty acid composition and markers of inflammation. Lipids. 2008 Jan;43(1):65-77.
Silverberg NB. Whey protein precipitating moderate to severe acne flares in 5 teenaged athletes. Cutis. 2012 Aug 1;90(2):70-2.
Melnik B. Dietary intervention in acne: attenuation of increased mTORC1 signaling promoted by Western diet. Dermatoendocrinol. 2012 Jan 1;4(1):20-32.
Jung GW, Tse JE, Guiha I, Rao J. Prospective, randomized, open-label trial comparing the safety, efficacy, and tolerability of an acne treatment regimen with and without a probiotic supplement and minocycline in subjects with mild to moderate acne. J Cutan Med Surg. 2013 Mar;17(2):114-22.
Dall’Oglio F, Milani M, Micali G. Effects of oral supplementation with FOS and GOS prebiotics in women with adult acne: The "SO Sweet" study: A proof-of-concept pilot trial. Clin Cosmet Investig Dermatol. 2018 Oct 8:445-9.
Chae M, Kim BJ, Na J, Kim SY, Lee JO, Kim YJ, Lee E, Cho D, Roh J, Kim W. Antimicrobial activity of Lactiplantibacillus plantarum APsulloc 331261 and APsulloc 331266 against pathogenic skin microbiota. Front Biosci Elite. 2021 Dec 20;13(2):237-48.
Kim J, Kim H, Jeon S, Jo J, Kim Y, Kim H. Synergistic antibacterial effects of probiotic lactic acid bacteria with Curcuma longa rhizome extract as synbiotic against Cutibacterium acnes. Appl Sci. 2020 Dec 15;10(24):8955.
Jung JY, Kwon HH, Hong JS, Yoon JY, Park MS, Jang MY, Suh DH. Effect of dietary supplementation with omega-3 fatty acid and gamma-linolenic acid on acne vulgaris: a randomized, double-blind, controlled trial. Acta Derm Venereol. 2014 Jan 29;94(5):521-5.
Steel A. Acne vulgaris. Clin Naturopathy Evid-Based Guide Pract. 2010 May 4:463.
Kaur I. Complementary and alternative medicine (CAM) in acne vulgaris. Res Clin Dermatol. 2018;1(1):18-19.
Ameya P, Nair PM. Role of therapeutic fasting along with other naturopathy and yoga modalities in addressing acne vulgaris—A single case report. J Nutr Fast Health. 2017 Sep 1;5(3):103-6.